Testicular cancer is a type of cancer that develops in the tissues of one or both testicles. If found early, testicular cancer can be cured.
There are two main types of testicular cancer:
Germ cell tumours are the most common types of testicular cancer, and there are two main types of these:
The Cancer Council estimates that more than ‘1,000 people were diagnosed with testicular cancer in 2023. The average age at diagnosis is 36 years old.’
Specific causes of testicular cancer are unknown, but some of the known risk factors include:
Testicular injuries, hot baths and tight clothes do not cause testicular cancer.
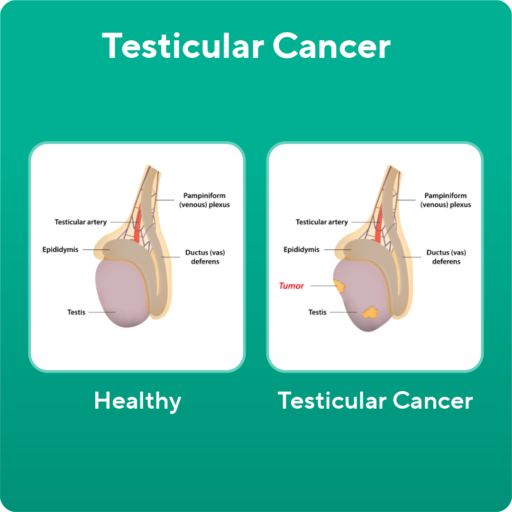
The most common symptoms of testicular cancer are:
In the early stages of the condition, you may notice no symptoms at all.
Some of the less common symptoms of testicular cancer may include:
If you notice lumps in one or both testicles, or changes in the shape of the testicle, visit your health care professional. They will conduct a physical examination and advise you on your next steps.
Testicular cancer is diagnosed through a combination of:
Importantly, testicular cancer can’t be diagnosed through a biopsy (taking a small sample to check for cancerous cells). Cutting into a testicle may risk spreading the cancer to other areas of the body.
In Australia, routine screening is not recommended for testicular cancer. However, if you have a known family history or genetic mutation, talk to your health care professional about yearly screening.
Treatment depends largely on the stage of the cancer. If you have testicular cancer, your medical team will determine the stage of the cancer and whether it has spread. To do this, you may need to have additional tests, such as a chest X-ray and CT scans of the chest, abdomen and pelvis.
The different stages of testicular cancer are:
The main treatment for stage 1 testicular cancer is to remove the testicle. This surgery is called an orchidectomy. If the cancer has spread to nearby organs, or certain features are seen within your tumour on microscopic examinations, other possible treatments include:
Stage 2 or 3 cancer is generally still managed with removal of the testicle to identify the type of tumour and guide specific therapy, but most cases are then managed with systemic chemotherapy. Following this, if there are residual masses, surgery or radiation may be appropriate.
Your cancer specialist can discuss the options in detail to determine the best treatment program for you.
If you have received a testicular cancer diagnosis, your medical team will give you a personalised treatment plan. It’s important to take the time to learn about your condition, treatments and future plan.
Connecting with other people who have cancer can help you to feel supported and not alone. A strong support network can be very beneficial for your emotional wellbeing, cancer management and treatment outcomes.
Your St Vincent’s cancer and men’s health teams will support you every step of the way.